How U.S. Health Care Came to Cost Insanely More
From H&HN Daily
Cost is the big factor. Cost is why we can't have nice things. The overwhelmingly vast pile of money we siphon into health care in the United States every year is the underlying driver of almost every other problem with health care in the United States from lack of access to waste to fragmentation to poor quality. We can't afford to fix the problems, cover everyone, do real outreach, build IT systems that are interoperable and transparent and doc-friendly — or so it seems, because at least on weak examination, every fix seems to add even more cost. And in the old ways of doing things in health care, the way we have been used to doing business, the conclusion of the weak examination has been correct: Despite the tsunami of money, there is never enough to do it right.
Health care that costs more than it needs to is not just an annoyance; it's a big factor in income inequality in the United States. The financial, physical and emotional burden of disease are major drivers of poverty. At the same time, the high cost of health care even after the Affordable Care Act means that many people don't access it when they need it, and this in turn deprives large swathes of the population of their true economic potential as entrepreneurs, workers and consumers. People who are burdened by disease and mental illness don't start businesses; don't show up for work; and don't spend as much money on cars, smartphones and cool apartments. Unnecessary sickness is a burden to the whole economy.
How did we get this way? What was the mechanism that differentiated U.S. health care from all other advanced countries? The usual suspects (such as "We have the most sophisticated research and teaching hospitals," or "It's the for-profit health insurers" or "Doctors make too much") all fail when we compare our system with other sophisticated national systems such as those in Germany and France. Other countries have all of these factors in varying amounts — private health insurers, world-class research, well-paid physicians — and cost a lot, but still spend a far smaller chunk of their economy on health care. Blame has been leveled in every direction but, in reality, no single part of health care has been the driver. The whole system has become drastically more expensive over the last three decades.
What's the Mechanism?
Since the difference between the United States and other countries is so large and obvious, there should be some way we can look at health care spending that would make that mechanism jump out at us. And there is a way.
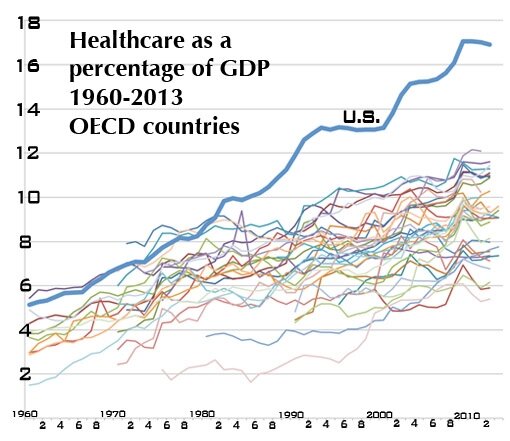
The Organization for Economic Cooperation and Development gathers and publishes huge amounts of information about the top 40 or so national economies in the world. Go online and search for its database on national health expenditures as a percentage of each country's economy. Don't just look for recent data. We already know what that says: The United States throws twice as large a chunk of its economy into health care as most other countries; 50 percent more than the most expensive other countries. No, take the search back to the middle of the last century. Pull the data into a spreadsheet. Make the spreadsheet into a graph. Here's what you get:
Wow. Suddenly a rather startling pattern emerges. Right side: Yes, the United States costs twice as much. Left side: Didn't use to.
As economies grow in absolute size, they tend to dedicate a greater percentage to health care. After a certain point, somewhere around 9 percent, the cost continues to increase, but the rate of increase tends to flatten somewhat. Through the '60s and '70s we can see that happening. The United States, as the largest economy, is one of the most expensive, but it's just there at the top of the pack. In the mid-1960s Medicare is implemented — the first big infusion of federal money into the health care economy — and does the U.S. line jump up? Not really. It flatlines for a year, then continues its moderate climb.
Something Wicked This Way Comes
Then something happens that is stark, sudden and large. Health care economies tend to lag national economies by a year or two; in bad economic times, governments and private purchasers can't cut health care expenditures immediately, but they do tighten their belts for the future. At a moment when the other most expensive health care economies (Germany, Sweden, Denmark) are flatlining or drifting lower in response to the global economic malaise of the early 1980s, the U.S. line goes nearly vertical, flatlines for a year or so, then leaps ever higher in a series of startling S-curves.
That first big leap is between 1982 and 1983. What was different in 1983 that was not there in 1982? DRGs, diagnosis-related groups — the first attempt by the government to control health care costs by attaching a code to each item, each type of case, each test or procedure, and assigning a price it would pay in each of the hundreds of markets across the country. The rises continue across subsequent years as versions of this code-based reimbursement system expand it from Medicare and Medicaid to private payers, from inpatient to ambulatory care, from hospitals to physician groups and clinics, to devices and supplies, eventually becoming the default system for paying for nearly all of U.S. health care: code-driven, fee-for-service reimbursements.
Cost Control Drives Costs Up?
How can a cost control scheme drive costs up? In a number of ways: In an attempt to control the costs of the system, the DRG rubric controlled the costs of units, from individual items like an aspirin or an arm sling to the most comprehensive items such as an operation or procedure. The system did not pay for an entire clinical case across the continuum of care from diagnosis through rehab; or for an entire patient per year on a capitated basis, which would capture the economic advantages of prevention; or for an entire population. While it is more cost-effective (as well as better medicine) to provide a diabetes patient with medical management, in-home nursing visits and nutritional counseling rather than, say, waiting until the patient needs an amputation, the coding system actually punished that efficiency and effectiveness. Under this system, we got paid for our inefficiencies, and even for our mistakes: Do-overs often would drop far more to the bottom line than the original procedure did.
The system punished, rather than rewarded, spending more time with patients, trying to help patients before their problems became acute, or maintaining a long-term, trusted relationship with patients. Under a code-driven, fee-for-service system, getting serious about prevention and population health management would be a broad road to bankruptcy.
If extra items were deemed necessary (an extra test or scan, say), there were codes for that, and reimbursements awaiting. In so doing, the system rewarded doing more (volume) rather than whatever would be the best, most appropriate, most efficient treatment path (value). It provided a written, detailed catalog of reimbursements which rewarded diagnoses of greater complexity, rewarded new techniques and technologies with new and usually higher reimbursements, and especially rewarded systems that invested in a greater capability to navigate the coding system. At the same time, the reimbursements were constantly open to pressure from the industry. Each part of the industry, each region, each specialty, each part of the device industry, became fiercely focused on keeping those reimbursements up, and getting new codes for more costly procedures.
The business and strategic side of health care became a matter of making money by farming the coding system. Do more of what gets better reimbursement, less of what does not. Make sure every item gets a code and gets charged for. The codes became a manual for success, a handbook for empire.
The Smoking Gun
The smoking gun is right there in the chart, at the big split between the trajectories of the United States and other countries. And today, at this moment, the code-based, fee-for-service payment system is still by far the basis of most revenue streams across health care.
The unifying factor between multiple new strategies unfolding in health care right now, including patient-centered medical homes, pay for performance, bundled prices, reference prices, accountable care organizations, direct pay primary care and others, is to find some way around the strict code-based, fee-for-service system, either by avoiding it entirely or by adding epicycles and feedback loops to it to counter its most deleterious effects.
There is no perfect way to pay for health care. All payment methods have their drawbacks and unintended consequences. But the code-based, fee-for-service system got us here, and any path out of the cost mess we are in has to get us off that escalator one way or another.
Joe Flower, CEO of the Change Project Inc., serves on Speakers Express, the speaking faculty of the AHA's Health Forum, and on the board of the Center for Health Design. He is also a regular contributor to H&HN Daily.
You can help MVHCA as we work for single payer health care by donating, hosting a house party, signing up for the newsletter, and attending our monthly meetings. You can also Like us on Facebook, and Follow us on Twitter. Thank you.